Uncovering Allergy Testing Part 1: What Tests Do I Need?
Allergists often say that history is the biggest determinant in diagnosing a patient’s allergies. However, specific allergy testing can also aid greatly in making the diagnosis. The La Crosse Method™ Protocol for allergy testing and treatment incorporates a variety of reproducible testing options that help the allergist get to the bottom of the allergy mystery in any given patient.
Dr. Mary Morris, partner at Allergy Associates of La Crosse (AAOL) and an author of the La Crosse Method™ Protocol, typically chooses between three different tests when seeing a patient. These three tests look for allergies in different ways.
Dr. Morris helps to explain the differences in tests and how they can benefit patients individually.
Skin Testing
Before testing begins — what you need to know
Skin testing for allergies has been used for over 100 years; it has been proven to be effective, non-invasive, and quick. Before arriving for a testing appointment, patients will be notified that certain medications must be limited before testing (for example, certain antihistamines and antidepressants).
Before testing begins, the doctor will conduct an exam and discuss the patient’s history. After this discussion, the doctor chooses allergens that could be potential culprits and testing is started — it’s not as scary as it sounds.
Intradermal skin testing

A small syringe is filled with an individual allergen and injected under the dermal layer of the skin. There are often 3-15 different allergen injections administered to the upper arm, depending on what was determined during the exam. Some patients relate the feeling to that of a mosquito bite.
Patients then wait 10 minutes for a reaction to occur, or not occur, on the skin. Each reaction is then measured with a small ruler and marked with a pen, and the size of the reaction is a telltale sign of how allergic the patient is to the inhalant allergen.
An additional benefit of the intradermal skin test is that it allows for the detection of delayed reactions. Some allergens, like molds, may take days to reach their full reaction. Looking for reactions days after the actual test and reporting these delayed reactions can be important indicators for doctors in determining the starting level of treatment. If delayed reactions are suspected, the doctor will often give the patient a “delay marker card” which will allow the patient to record and report any delayed reactions that he/she observed one and two days after testing.
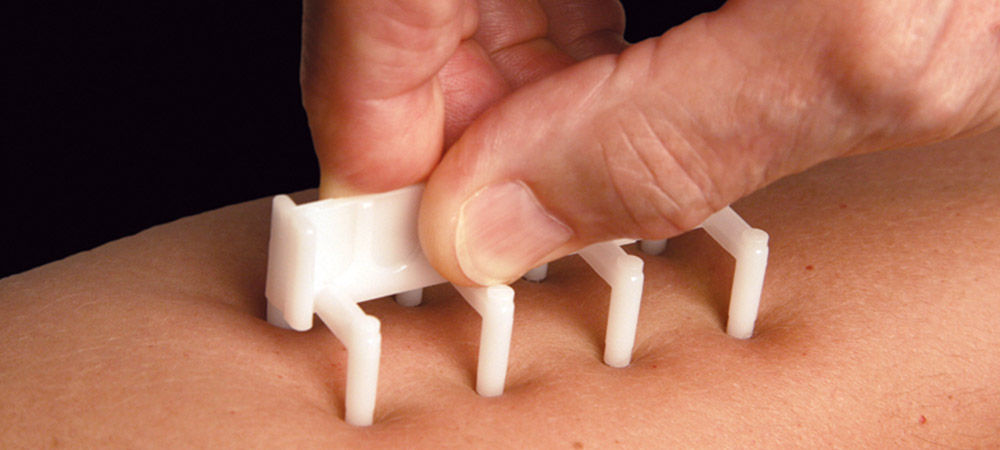
Skin prick testing

Results are found after 15 minutes in the same way as with intradermal testing, by measuring the “wheals” or reactions with a small ruler. A second measurement is taken, though, as the surrounding redness is measured separately, along with the wheal size.
“Skin prick testing for foods has more false positives, but it has very few false negative tests. So, we’ve been using it a lot to rule out reactivity to certain foods,” Dr. Morris states. “It’s also something that is required before we do a graded oral food challenge at our clinic.”
Allergy drops can be prescribed for identified allergies after this test, too!
Blood Testing

This test is also particularly helpful in young children and infants, where multiple skin tests with needles are impractical due to small arm area and potential discomfort.
Like skin testing, a history and exam are completed to decide what should be tested. The procedure itself is identical to any other blood test, simply drawing a vial of blood from a ready vein to detect food and inhalant allergies.
When the blood goes to the lab, the magic happens. The blood sample is assessed for a specific allergy antibody — termed IgE — to specific inhalants and/or foods. It’s scientific and complex, but a number of labs show validated results that prove accurate. Stay tuned for part two of this blog to understand more about IgE and how allergenicity is determined with a blood test.
Post-Test
After testing, precise, individually-tailored allergy drops can be prescribed to treat the root cause of the allergy. Allergy drops work similarly to allergy shots to help build long-term tolerance to the offending allergen. While you may be a bit itchy from skin testing, or have an annoying band aid after blood testing, you will leave with the satisfaction of knowing that the treatment you’re given is one that can help you reduce allergy symptoms for years to come.
Check out Allergychoices conditions best treated page for more information on what conditions can be treated with allergy drops.
Treat the Cause
Interested in learning how personalized allergy drop immunotherapy can be used to treat the cause of your allergies? Find a provider near you who has received training and currently reports following the La Crosse Method Protocol for allergy drop immunotherapy.

